
Quick Guide to Medicaid
In Triage Health's free Quick Guide to Medicaid, learn about what Medicaid is called in different states, how to qualify, how Medicaid and Medicare can work together, how and when to apply for Medicaid, what Medicaid covers, what it costs, appealing denials of coverage, and moving and Medicaid.
Medicaid is a federal program that provides free or low-cost health insurance coverage to certain individuals. Medicaid is the largest source of health coverage in the country, covering more than 88 million people.
Even though Medicaid is a federal program, it is run at the state level. Medicaid is funded at the federal and state level. The federal government requires all states to provide a minimum level of benefits, but states are allowed to apply for exceptions. So, while Medicaid programs must follow federal rules, the coverage, costs, and other details may be different in each state. For example, Medicaid programs have different names.
| State | Name of Medicaid Program |
|---|---|
| AK | Medicaid |
| AL | Medicaid |
| AR | Arkansas Medicaid |
| AZ | Arizona Health Care Cost Containment System |
| CA | Medi-Cal |
| CO | Health First Colorado |
| CT | Connecticut Medicaid (Husky Health) |
| DE | Medicaid |
| FL | Florida Medicaid |
| GA | Georgia Medical Assistance |
| HI | Med Quest |
| ID | Medicaid |
| IL | Illinois Medicaid |
| IN | Indiana Medicaid |
| IA | Iowa Medicaid |
| KS | KanCare program |
| KY | Kentucky Medicaid |
| LA | Health Louisiana |
| ME | MaineCare |
| MD | Maryland Medicaid |
| MA | MassHealth |
| MI | Michigan Medicaid |
| MN | Minnesota Medical Assistance |
| MS | Mississippi Medicaid |
| MO | MO HealthNet |
| NE | Medicaid |
| NV | Medicaid |
| NH | New Hampshire Medicaid |
| NJ | New Jersey FamilyCare |
| NM | Medicaid |
| NY | Medicaid |
| NC | North Carolina Medicaid |
| ND | Medicaid |
| OH | Ohio Medicaid |
| OK | SoonerCare |
| OR | Oregon Health Plan |
| PA | Pennsylvania Medical Assistance |
| RI | Rhode Island Medical Assistance |
| SC | Healthy Connections |
| SD | Medicaid |
| TN | TennCare |
| TX | Medicaid |
| UT | Medicaid |
| VT | Vermont Medicaid |
| VA | Medicaid |
| WA | Apple Health (Medicaid) |
| WV | West Virginia Medicaid |
| WI | BadgerCare Plus |
| WY | Medicaid |
| DC | DC Medicaid |
How to Qualify
In all states, Medicaid is available to people with a low income, low resources, and meet a specific category of eligibility. Those categories are different in each state, but usually include:
- Children
- Pregnant women
- Seniors, and
- People with disabilities who are receiving Supplemental Security Income (SSI).
Resources are things like money in a bank account or retirement account, like a 401k plan.
These different categories of eligibility are like different doors into the Medicaid program. Some doors require that you have a low income and resource level, while the Medicaid expansion door only requires that you have a low income.
States may have different rules on what income level you must have to get in certain doors. For example, if you have a disability, you may need to have an income level below 100% of the federal poverty level (FPL). If you are a child, your family income may need to be below 250% of the FPL.
States may also have their own special doors to get into the Medicaid program. For example, Minnesota and New York also give individuals with a household income between 138-200% FPL access to Medicaid through the Basic Health Program.
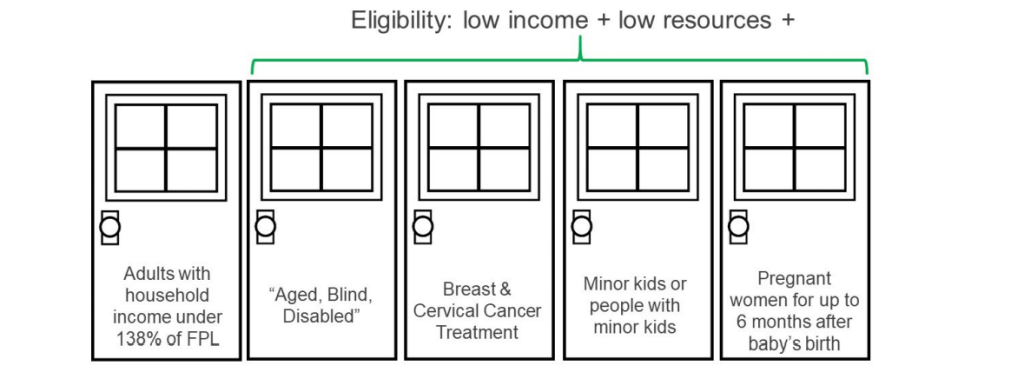
Since 2014, 41 states have expanded Medicaid to people with a household income under 138% of the federal poverty level ($21,597 in 2025), creating a new door into Medicaid. In these states, Medicaid will only look at your income to see if you qualify for this program, not your resources. This is called Medicaid expansion.
See the chart below to see if your state has expanded Medicaid.
| Household Size | 138%* |
|---|---|
| 1 | $21,597 |
| 2 | $29,187 |
| 3 | $36,777 |
| 4 | $44,367 |
| 5 | $51,957 |
| 6 | $59,547 |
| Expanded: 41 | Not Expanded: 10 |
|---|---|
| AK, AR, AZ, CA, CO, CT, DC, DE, HI, IA, ID, IL, IN, KY, LA, MA, MD, ME, MI, MN, MO, MT, NC, ND, NE, NH, NJ, NM, NV, NY, OH, OK, OR, PA, RI, SD, UT, VA, VT, WA, WV | AL, FL, GA, KS, MS, SC, TN, TX, WI, WY |
Medicaid and Medicare
If you are over the age of 65, or if you are receiving Social Security Disability Insurance (or SSDI) benefits, then you may also be eligible for Medicare. Medicare is another federal health insurance program for seniors and people with disabilities. If you qualify for both programs, Medicare typically is the primary payer. Medicaid can help pay for things Medicare doesn’t pay for (e.g., dental care in some states), and lowers out-of-pocket costs for Medicare Parts A and B. States can also pay premiums for Medicare Advantage (MA) plans.
When & How to Apply
You can apply for Medicaid at any time. You can apply online at HealthCare.gov, or through your state Medicaid agency.
Your Medicaid coverage will start usually start on the day that you apply, or on the first day of the month that you apply. Some states will also go back three months before you applied, to pay for any medical care that you received. If you stop being eligible for Medicaid, your coverage will usually end at the end of that month.
There are two types of Medicaid plans: fee-for-service plans and managed care plans.
- Fee-for-service plans allow you to see any health care provider who accepts Medicaid.
- Managed care plans require you to use a specific set of health care providers who are in the plan’s network.
Depending on the state and county that you live in, you may have access to fee-for-service plans, managed care plans, or both.
What MUST Medicaid Cover
In every state, Medicaid covers medical care that you receive in a hospital, or outside of a hospital, like going to visit your doctor. It also covers things like blood tests, x-rays, and scans. It covers care when you are pregnant, as well as mental health care. Medicaid also pays for long-term care services. Medicaid must also cover routine costs when you participate in a clinical trial.
- Inpatient hospital services
- Outpatient hospital services
- Physician services
- Laboratory and X-ray services
- Transportation to medical care
- Family planning services
- Home health services
- Nurse Midwife services
- Certified Pediatric and Family Nurse Practitioner services
- Freestanding Birth Center services (when licensed or otherwise recognized by the state)
- EPSDT: Early and Periodic Screening, Diagnostic,
and Treatment Services - Nursing Facility Services
- Rural health clinic services
- Federally qualified health center services
- Tobacco cessation counseling for pregnant women
What Medicaid May Cover
- Prescription Drugs
- Physical therapy
- Podiatry services
- Optometry services
- Dental Services (Adults)
- Dentures
- Prosthetics
- Personal Care
- Hospice
- Eyeglasses
- Chiropractic services
- Occupational therapy
- Speech, hearing, and language disorder services
- Respiratory care services
- Case management
- Other diagnostic, screening, preventive and rehabilitative services
- Other practitioner services
- Clinic services
- Private duty nursing services
- Services for Individuals Age 65 or Older in an Institution for Mental Disease (IMD)
- Services in an intermediate care facility for Individuals with Intellectual Disabilities
- State Plan Home and Community Based Services- 1915(i)
- Self-Directed Personal Assistance Services- 1915(j)
- Community First Choice Option- 1915(k)
- TB Related Services
- Inpatient psychiatric services for individuals under age 21
- Other services approved by the Secretary*
*This includes services furnished in a religious nonmedical health care institution, emergency hospital services by a non-Medicare certified hospital, and critical access hospital (CAH).
What Medicaid Costs
What you pay each month for Medicaid depends on the state that you live in and how you qualify for Medicaid. You may also have to pay certain costs out-of-pocket. For example, a co-payment is a fixed dollar amount that you have to pay when you get certain types of medical care. So, if you need a prescription drug, you may have to pay a co-payment at the pharmacy.
- Prescription Drugs: States can charge more for prescription drugs. Co-payments are different for generic versus brand-name drugs, or preferred drugs. For those above 150% FPL, co-payments for non-preferred drugs may be as high as 20% of the drug cost. For those at or below 150% FPL, co-payments are limited to small, fixed amounts (e.g., $3). Co-payments for mail-order drugs and drugs sold in a pharmacy are also different.
When & How to Appeal Denials
If you receive a claim denial or a denial of Medicaid eligibility, you have the right to appeal. The details of the appeals process may depend on where you live and whether you have fee-for-service Medicaid or a Medicaid managed care plan, but generally, you must file an appeal within 90 days of receiving the Notice of Action (NOA). If you file within 10 days, you may continue to receive benefits while your appeal is pending. You should contact the Medicaid Office where you live (or where you lived when you received the services). If you need help with a Medicaid appeal, you can contact a local legal aid organization that handles Medicaid or government benefits cases.
Moving with Medicaid
Because each state operates its own Medicaid program and has different rules, you cannot transfer your Medicaid coverage from one state to another, and you cannot have Medicaid coverage in two states at the same time. But if you are moving to a new state, it is important to:
- Learn about the eligibility rules in your new state, because they may be different from where you live now. Contact your new state’s Medicaid agency.
- Look to see how Medicaid benefits in your new state compare to your current benefits. For example, your new state may offer more or fewer optional benefits, such as dental coverage.
- Talk to your health care team to let them know you are considering moving, as they may be able to help with the transfer of your medical care and your Medicaid coverage.
- Plan ahead, to avoid a gap in your coverage. Because most states end existing Medicaid coverage at the end of the month, the best way to prevent a lapse is to move close to the end of the month, cancel your coverage in your original state, and immediately apply for coverage in your new state. On average, it takes 7 to 90 days for Medicaid applications to be processed by a state.
Where to Go for Help
Contact your state Medicaid agency for help with:
- Medicaid Eligibility and Status of a Medicaid/CHIP Application
- Medicaid Claims, Coverage, and Services
- Lost Medicaid Card/Replacement
- Finding a Medicaid/CHIP Provider
To find the contact information for your state’s Medicaid agency visit TriageHealth.org/State-Resources.
Learn More
For more information about Medicaid and other health insurance options,
visit TriageHealth.org/Health-insurance or CancerFinances.org.
Sharing Our Quick Guides
We're glad you found this resource helpful! Please feel free to share this resource with your communities or to post a link on your organization's website. If you are a health care professional, we provide free, bulk copies of many of our resources. To make a request, visit TriageHealth.org/MaterialRequest.
However, this content may not be reproduced, in whole or in part, without the express permission of Triage Cancer. Please email us at TriageHealth@TriageCancer.org to request permission.
Last reviewed for updates: 02/2025
Disclaimer: This handout is intended to provide general information on the topics presented. It is provided with the understanding that Triage Cancer is not engaged in rendering any legal, medical, or professional services by its publication or distribution. Although this content was reviewed by a professional, it should not be used as a substitute for professional services. © Triage Cancer 2025
